Saccular cerebral aneurysms, also known as berry aneurysms, are the most common type of intracranial aneurysms. These rounded, bulging formations in the walls of cerebral arteries account for the vast majority of non-traumatic subarachnoid hemorrhages – a life-threatening condition requiring prompt medical intervention.
Anatomy and Pathophysiology
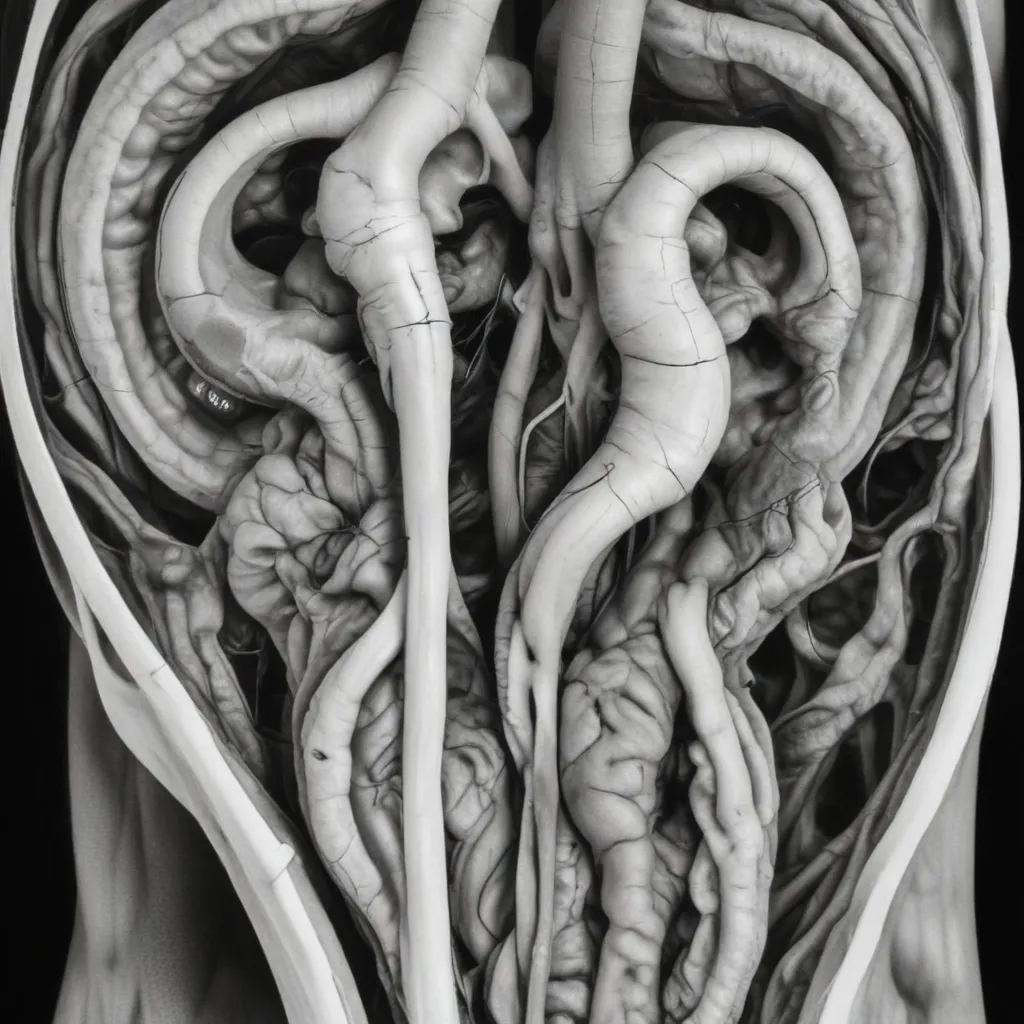
A saccular aneurysm refers to a focal, spherical dilation of an artery, usually occurring at a branching point or curve in the vessel. In contrast, a fusiform aneurysm involves a more gradual, spindle-shaped expansion of the entire arterial circumference. Saccular aneurysms are the predominant form, comprising around 90% of all cerebral aneurysms, while fusiform aneurysms are more common in the aorta.
The development of saccular aneurysms is a multifactorial process, primarily driven by degenerative changes in the arterial wall. Key factors include:
- Hemodynamic stress: Turbulent blood flow and increased shear stress at arterial bifurcations can lead to focal weakening of the vessel wall.
- Inflammation: Inflammatory mediators like T-cells and macrophages may contribute to structural deterioration.
- Congenital defects: Inherited collagen disorders or deficiencies in the internal elastic lamina can predispose to aneurysm formation.
These factors culminate in disruption of the normal arterial architecture, particularly the media layer, leaving the vessel vulnerable to outpouching and ballooning under hemodynamic forces.
A third type, the mycotic aneurysm, arises from infectious processes that weaken the arterial wall, often due to bacterial or fungal invasion. These aneurysms are less common but can still result in devastating complications.
Epidemiology and Risk Factors
Saccular cerebral aneurysms have an estimated prevalence of 3.2-4% in the general population, with a mean age of presentation around 50 years. Women are slightly more affected than men, especially after age 50.
Modifiable risk factors for saccular aneurysm development and rupture include:
- Hypertension: Chronic elevated blood pressure accelerates arterial degeneration.
- Smoking: Nicotine exposure impairs vascular smooth muscle function.
- Excessive alcohol consumption: Can contribute to hypertension and weaken the arterial wall.
Non-modifiable risk factors include:
- Family history: First-degree relatives face a 3-7 times higher risk.
- Genetic disorders: Conditions like polycystic kidney disease, Marfan syndrome, and Ehlers-Danlos syndrome predispose to aneurysm formation.
- Race: African Americans exhibit a higher incidence compared to other ethnicities.
The annual rupture risk for unruptured saccular aneurysms ranges from 1-2%, with larger and posterior circulation aneurysms posing a greater danger.
Imaging Modalities
Several imaging techniques are utilized to diagnose and evaluate cerebral aneurysms:
Computed Tomography Angiography (CTA): A rapid, widely available method that can accurately visualize the aneurysm size, neck, and relationship to surrounding vessels.
Magnetic Resonance Angiography (MRA): Provides high-resolution, non-invasive imaging without ionizing radiation, though small aneurysms may be missed.
Digital Subtraction Angiography (DSA): Considered the gold standard, this catheter-based technique offers exquisite detail of the vascular anatomy and is particularly useful for assessing aneurysm morphology.
Emerging modalities like contrast-enhanced MRI targeting inflammatory biomarkers may further refine the detection of high-risk aneurysms prone to rupture.
Clinical Presentation and Diagnosis
The majority of saccular cerebral aneurysms (85-90%) are asymptomatic and incidentally discovered during imaging for unrelated reasons. However, warning signs include:
Unruptured aneurysms:
– Headaches, dizziness, or vision changes
– Cranial nerve palsies from mass effect
Ruptured aneurysms:
– Sudden, severe “thunderclap” headache
– Nausea, vomiting, and neck stiffness
– Altered mental status or focal neurological deficits
The initial diagnostic test for suspected subarachnoid hemorrhage is a non-contrast head CT scan, which is 100% sensitive within 6 hours of symptom onset. If the CT is negative but clinical suspicion remains high, a lumbar puncture is performed to assess for xanthochromia – a yellowish discoloration of the cerebrospinal fluid due to hemoglobin breakdown.
Once the diagnosis of subarachnoid hemorrhage is established, further vascular imaging with CTA, MRA, or DSA is needed to identify the culprit aneurysm and guide treatment.
Management and Treatment
The management of saccular cerebral aneurysms depends on several factors, including the patient’s age, medical history, aneurysm size and location, and whether rupture has occurred.
Unruptured aneurysms:
– Small (< 7 mm), incidental aneurysms in older patients may be observed with periodic imaging surveillance.
– Larger, symptomatic, or high-risk aneurysms typically warrant intervention to prevent rupture.
Ruptured aneurysms:
– Urgent treatment, either endovascular coiling or surgical clipping, is essential to prevent rebleeding and improve outcomes.
– Additional management includes maintaining optimal blood pressure, monitoring for vasospasm, and managing hydrocephalus or other complications.
Endovascular coiling: A minimally invasive procedure where platinum coils are deployed within the aneurysm sac to induce thrombosis and seal off the defect.
Surgical clipping: Open craniotomy to directly visualize and clip the aneurysm neck, isolating it from the parent artery.
The choice between endovascular and surgical approaches depends on the aneurysm characteristics, patient factors, and the expertise of the treating team.
Complications and Prognosis
The primary concern with saccular cerebral aneurysms is the risk of rupture, leading to devastating subarachnoid hemorrhage. Approximately 10-30% of patients do not survive long enough to reach the hospital, and only about 30% of those who do make a good recovery.
Complications of ruptured aneurysms include:
- Rebleeding: A major cause of morbidity and mortality in the first 48 hours, with a 20-50% risk if untreated.
- Cerebral vasospasm: Constriction of cerebral arteries, causing delayed cerebral ischemia and infarction, typically occurring 3-14 days after the initial hemorrhage.
- Hydrocephalus: Accumulation of cerebrospinal fluid, leading to increased intracranial pressure.
The overall prognosis for patients with ruptured saccular aneurysms remains guarded, with mortality rates ranging from 25-50% and a high risk of permanent neurological deficits in survivors.
Preventive Strategies
Given the serious consequences of saccular cerebral aneurysm rupture, prevention and early detection are crucial. Key strategies include:
Lifestyle modifications:
– Smoking cessation
– Alcohol moderation
– Blood pressure control
Screening and surveillance:
– Routine imaging for high-risk individuals (family history, genetic conditions)
– Regular follow-up for known unruptured aneurysms
By addressing modifiable risk factors and implementing appropriate screening protocols, clinicians can help mitigate the burden of this potentially life-threatening vascular disorder. Early detection and timely intervention are essential for optimizing patient outcomes.
For more information, please visit www.winegardeninn.com to explore our comprehensive resources on culinary delights, food & wine pairings, garden tips, wine & health, wine education, and our winemaking journey.